A novel strategy with the potential to treat many diseases including cancer is known as immunotherapy. It is a new and promising option for modern medicine, Immunotherapy is a cutting-edge departure from conventional therapies that enables the body’s immune system to launch a defense.
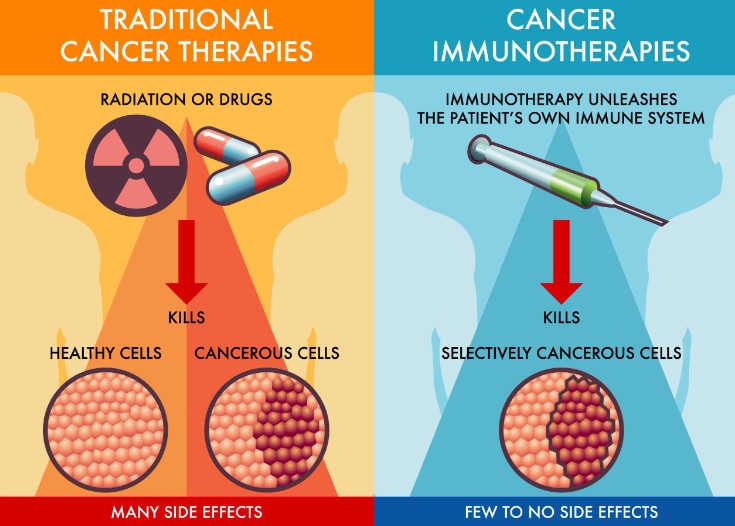
The body’s defense mechanism against harmful invaders such as viruses, bacteria and abnormal cells is the immune system. However, cancer cells often cunningly evade detection by the immune system, enabling them to spread without restraint. Immunotherapies work by enhancing or restoring the immune system’s function, allowing it to identify cancerous cells as targets for destruction. But it is important to note that immunotherapy will not be a one size fits all solution and the success of these treatments are dependent on many factors including the type of cancer, the patient’s overall health status and special immunotherapy applied.
Researchers and medical experts continue to seek new treatment options for diseases like autoimmune disorders and infectious diseases as the field of immunotherapy develops.
The Immune System’s Role in Cancer Defense
- Surveillance and Detection: When a cell undergoes mutations and becomes cancerous, it may display specific markers or antigens that differentiate it from normal cells. The ability of the immune system to detect this anomaly is an essential initial step in protecting against cancer.
- Natural Killer (NK) Cells: NK cells have the unique ability to identify cancerous cells by detecting changes in their surface proteins. Once detected, NK cells release toxic substances that induce programmed cell death in the cancer cells.
- The Immune Warriors: There are two primary types of T cells involved in cancer immunity: helper T cells (CD4+) and cytotoxic T cells (CD8+). Helper T cells assist in coordinating the immune response, while cytotoxic T cells are directly responsible for attacking and destroying cancer cells.
- Dendritic Cells: Dendritic cells resemble the immune system’s messengers. They collect tumor antigens and pass them on to T cells, effectively “educating” the T cell against the cancer.
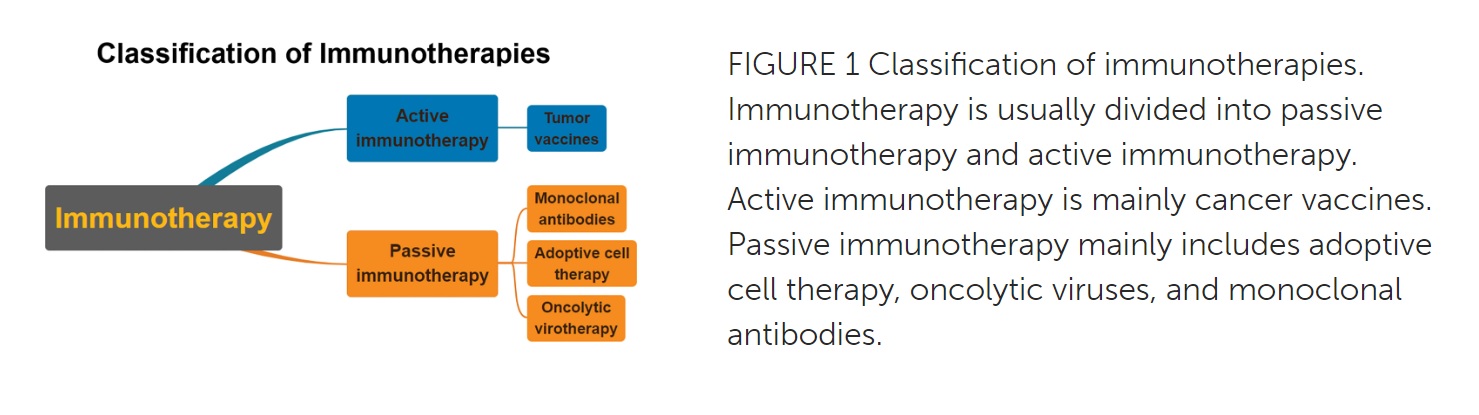
Types of Immunotherapy
- Checkpoint Inhibitors: Classes of medicines known as checkpoint inhibitors, which play an important role in the treatment of cancer are included in immunotherapies. These inhibitors function by targeting specific immune checkpoints—molecules on the surface of immune cells—responsible for regulating the intensity and duration of immune responses. These checkpoints are used by cancer cells, which allow them to evade detection of and elimination of the immune system.
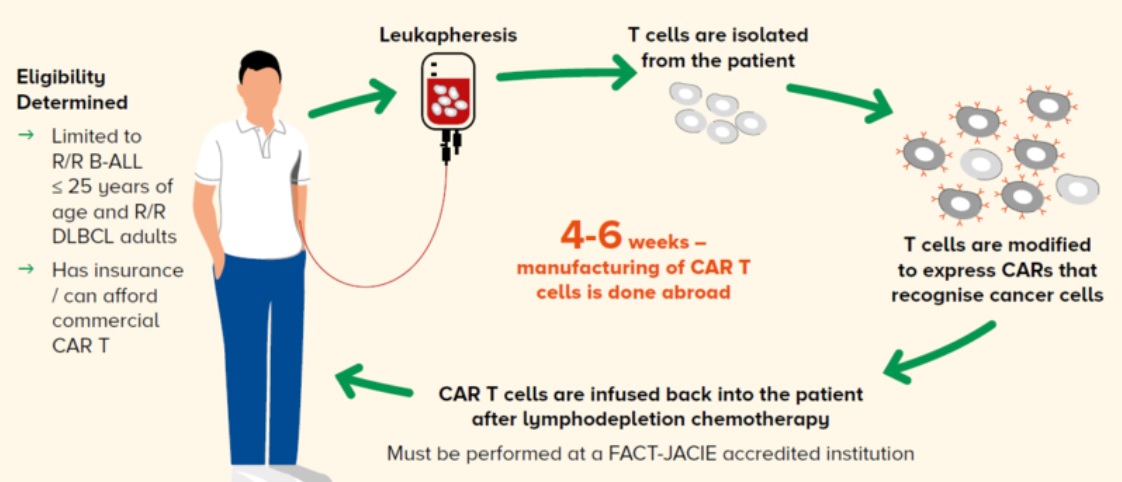
- Adoptive Cell Therapies: This involves extracting T cells—specialized immune cells—from the patient’s body. Subsequently, these T cells undergo meticulous engineering and reprogramming in vitro to equip them with enhanced cancer cell recognition capabilities. Once suitably armed, the modified T cells, now referred to as chimeric antigen receptor (CAR) T cells or tumor-infiltrating lymphocytes (TILs), are then infused back into the patient. The infused T cells launch a targeted and vigorous assault against cancer cells.
- Cancer Vaccines: Unlike conventional vaccines that prevent infectious diseases, cancer vaccines aim to prime the immune system to recognize and respond to specific cancer-associated antigens. While cancer vaccines are still in the early stages of development, they hold substantial promise as a potential preventive measure for cancer treatment.
- Immune System Modulators: Immune system modulators are a diverse group of substances such as cytokines and immune stimulators which are used to regulate and fine-tune the immune response.
These modulators are substances that can fight cancer, infectious diseases and conditions where the body’s immune system attacks it. They provide new and better treatment choices for patients leading to improved results and outcomes.
Promising Outcomes of Immunotherapy in Cancer Treatment
- Melanoma: Immunotherapy has shown remarkable success in treating advanced melanoma, a type of skin cancer. Some patients with metastatic melanoma have experienced durable responses and long-term survival after receiving immune checkpoint inhibitors such as pembrolizumab or nivolumab.
- Lung cancer: Immunotherapy for NSCLC is promising during the treatment of non SCCL. Some patients with advanced NSCLC and high PD-L1 expression have responded well to immune checkpoint inhibitors, leading to prolonged survival.
- Leukemia: Chimeric Antigen Receptor (CAR) T-cell therapy, a form of adoptive cell therapy, has shown significant success in certain types of leukemia. To treat and destroy cancer cells, CAR T cell therapy requires the production of a patient’s T cells by genetic engineering. Some patients with relapsed or refractory leukemia have achieved emission and long-term disease control after CAR T-cell therapy.
- Lymphoma: Immune checkpoint inhibitors have shown promising results in certain types of lymphoma, particularly Hodgkin lymphoma. Patients who have failed previous treatments or relapsed have achieved remissions and prolonged survival with immunotherapy.
- Bladder cancer: Immune checkpoint inhibitors have demonstrated efficacy in the treatment of advanced or metastatic bladder cancer. Some patients with advanced bladder cancer have experienced tumor shrinkage and improved overall survival after receiving immunotherapy.
Potential for Treating Other Conditions Beyond Cancer
- Autoimmune diseases: Immunotherapy is being investigated as a potential treatment for autoimmune diseases, such as rheumatoid arthritis, multiple sclerosis, psoriasis, and lupus. By modulating the immune response, researchers aim to control the overactive immune system responsible for attacking healthy tissues.
- Antiviral Immunotherapy: Immunotherapies are designed to boost immune response in case of infection with viruses. It also includes monoclonal antibodies, which are specifically capable of binding to a specific virus protein and preventing it from entering host cells. Monoclonal antibodies were produced and approved for use in a variety of viral infections including Respiratory Syncytial virus RSV9 and Human Immunodeficiency Virus RSV9.
- Infectious diseases: Immunotherapy is being explored as a strategy to treat bacterial, and parasitic infections. This includes using immune-based therapies to enhance the body’s ability to fight infections or developing vaccines to prevent certain infectious diseases.
- Allergies: Allergen-specific immunotherapy, commonly known as allergy shots, is a well-established form of immunotherapy to treat allergies. It helps desensitize the immune system to specific allergens, reducing the severity of allergic reactions over time.
- Organ transplantation: Immunotherapy is used to prevent organ rejection in transplant patients. Immunosuppressive drugs are commonly used to reduce the immune response against the transplanted organ and improve the chances of successful transplantation.
- Chronic inflammatory conditions: In conditions like inflammatory bowel disease (IBD) and asthma, researchers are exploring immunotherapy approaches to regulate the inflammatory response and alleviate symptoms.
- Neurological disorders: Immunotherapy is being investigated for certain neurological disorders, such as Alzheimer’s disease, where targeting specific proteins or immune responses may slow down disease progression.
- Hematological disorders: Immunotherapy is utilized in treating certain blood disorders, including aplastic anemia and certain types of hemophilia.
- Diabetes: Immunotherapy is being researched as a potential treatment for type 1 diabetes aiming to stop or slow down the autoimmune destruction of insulin-producing cells in the pancreas.
It’s important to note that while immunotherapy has shown promise in these areas, many of these applications are still in the early stages of research and development. The immune system is a complex network and fine-tuning it for specific conditions can be challenging. Additionally, the safety and efficacy of immunotherapy in these contexts may vary and require further study.
Immunotherapy: Steps to Determine Eligibility
Becoming a candidate for immunotherapy involves a thorough evaluation by healthcare professionals to determine if this treatment approach is suitable for your specific medical condition. Here are some general steps that may be involved in determining eligibility for immunotherapy:
- Diagnosis and Cancer Type: The first step is a proper diagnosis of your medical condition, which includes identifying the type and stage of cancer or other diseases.
- Biomarker Testing: Biomarker testing involves analyzing specific molecules or genetic markers in your tumor tissue or blood. Some immunotherapies are targeted to work better in patients with certain biomarkers, such as PD-L1 expression or microsatellite instability (MSI). These tests help predict the likelihood of response to immunotherapy.
- Medical History and Overall Health: Your healthcare team will review your medical history, including previous treatments and any other medical conditions you may have. They will also assess your overall health and functional status to determine if you can tolerate immunotherapy.
- Stage of Disease: Immunotherapy is typically more effective in advanced or metastatic cancers, but it may also be considered for earlier stages in certain cases.
- Performance Status: Your performance status, a measure of your ability to perform daily activities, is considered when evaluating your eligibility for immunotherapy. Patients with good performance status are generally better candidates for this treatment.
- Clinical Trial Participation: If you are not eligible for standard immunotherapy or other treatments, your healthcare team may discuss the possibility of participating in clinical trials that are testing new or experimental immunotherapy treatments.
It’s essential to have an open and honest discussion with your healthcare provider about your treatment options, including the potential benefits and risks of immunotherapy. Each patient’s situation is unique, and the decision to undergo immunotherapy should be made collaboratively between you and your healthcare team.
Understanding Why Some Patients Do Not Respond Well To Immunotherapy
- Tumor Microenvironment: Tumors can create a hostile microenvironment that dampens the immune response. They release immunosuppressive factors and attract regulatory immune cells, which impair the ability of the immune system to recognize and attack cancer cells.
- Lack of Target Antigens: Immunotherapies rely on the immune system recognizing specific antigens on cancer cells. If the tumor lacks these target antigens, the immune response may not be activated effectively.
- Tumor Heterogeneity: Tumors can consist of various cell types with different genetic characteristics and immune properties. In some cancer cells, the antigens they are targeting may not be expressed.
- Inadequate T-cell Infiltration: Tumors can actively resist the immune cells responsible for attacking cancer cells. This limits the immune system’s access to the cancer cells and hampers the response to immunotherapy.
- Genetic Alterations: Genetic mutations within the tumor can disrupt antigen presentation pathways or other immune-related mechanisms, making the tumor less vulnerable to immune attack.
- Pre-existing Immune Tolerance: In some cases, the immune system may already be tolerant to the tumor antigens, resulting in limited or no immune response when treated with immunotherapy.
- Patient-specific Factors: Individual patient factors, such as overall health, immune status, and genetic makeup, can influence the response to immunotherapy.
Creating solutions to these problems requires an understanding of the causes of immunological resistance. Researchers are exploring combination therapies; personalized treatments tailored to each patient’s specific tumor characteristics and improve outcomes for patients.
Common Side Effects Of Immunotherapy Treatment
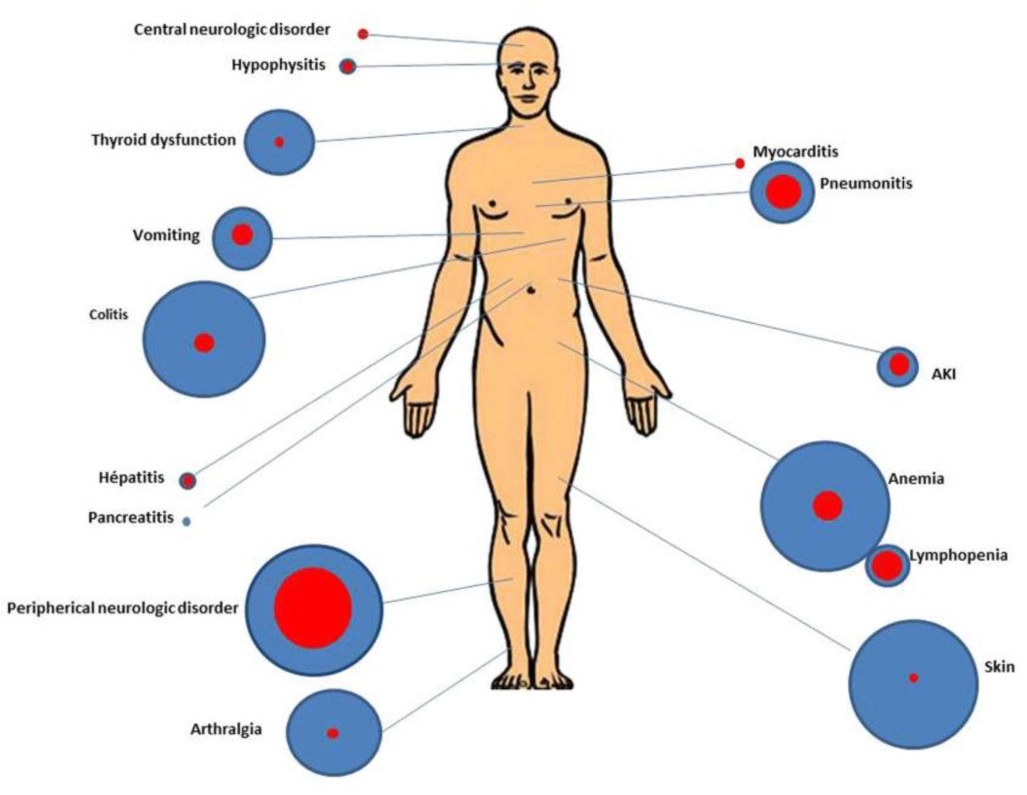
Immunotherapy has revolutionized cancer treatment, but it can also cause a range of side effects. The side effects vary depending on the type of immunotherapy, the specific drug used, the individual’s overall health and the type of cancer being treated. Some of the common side effects of immunotherapy treatments include:
- Fatigue: Feeling tired or weak is a common side effect of immunotherapy. It may be mild or severe and can affect daily activities.
- Skin reactions: Immunotherapy can cause skin-related side effects, such as rashes, itching, or blistering. In some cases, patients may develop a condition called “dermatitis” or “dermatitis-like rash.”
- Gastrointestinal issues: Diarrhea, nausea, vomiting, and loss of appetite are common gastrointestinal side effects of immunotherapy.
- Flu-like symptoms: Some patients may experience flu-like symptoms, including fever, chills, muscle aches, and headache.
- Respiratory problems: Immunotherapy drugs can sometimes cause coughing, shortness of breath, or other respiratory issues.
- Endocrine-related side effects: Certain immunotherapy drugs can affect the endocrine system, leading to thyroid problems, adrenal gland issues, or changes in blood sugar levels.
- Liver problems: Immunotherapy may cause liver enzyme abnormalities or hepatitis-like symptoms.
- Immune-related adverse events (irAEs): Immunotherapy involves stimulating the immune system which can lead to autoimmunity-like reaction in different organs such as skin, lungs, intestines and endocrine glands.
- Infusion reactions: Some patients may experience infusion-related reactions during or shortly after receiving the immunotherapy infusion.
Frequently Asked Questions On Immunotherapy
What types of cancers can be treated with immunotherapy?
Immunotherapy has shown promise in treating various types of cancer. Some cancers that have demonstrated significant responses to immunotherapy include melanoma (a type of skin cancer), lung cancer, bladder cancer, lymphoma, leukemia and certain types of gastrointestinal and head and neck cancers. Research is ongoing to explore its potential in other cancer types as well.
Is immunotherapy a replacement for traditional cancer treatments like chemotherapy and radiation therapy?
Immunotherapy is not always a replacement for traditional cancer treatments like chemotherapy or radiation therapy. In many cases, it is used in combination with these treatments to achieve better outcomes. Combinations of immunotherapy with traditional therapies have shown synergistic effects leading to improved response rates and prolonged survival in certain cancers.
How long does immunotherapy treatment typically last?
The duration of immunotherapy treatment can vary depending on the cancer type, stage, treatment response, and the specific immunotherapy used. In some cases, immunotherapy may be administered for a set number of cycles or a defined period. For other patients with sustained responses, it may continue for an extended duration.
How effective is immunotherapy compared to other cancer treatments?
Immunotherapy has demonstrated impressive effectiveness in certain cancers, often providing durable responses and improved overall survival compared to traditional treatments. However, the extent of effectiveness can vary depending on the cancer type, stage, and the individual’s immune response.
Are there any lifestyle changes that can enhance the effectiveness of immunotherapy?
Leading a healthy lifestyle can positively impact the effectiveness of immunotherapy. Maintaining a balanced diet, regular exercise, managing stress, avoiding smoking and excessive alcohol consumption can help support the immune system’s response to treatment. To ensure their appropriateness for your situation, lifestyle changes should be discussed with your healthcare team.
Can pediatric tumors be treated with immunotherapy?
Yes, in the treatment of childhood cancer, immunotherapies are also investigated and applied. Some immunotherapy drugs such as checkpoint inhibitors have shown promise in certain pediatric cancers like neuroblastoma and certain types of brain tumors. However, studies in this area are still being carried out and decisions on the treatment of pediatric tumors are based upon cases.